It’s been over three years for David Israel, who first noticed a small protruding lump on each side of his face in June of 2015. Three days after seeing the doctor about the lumps, he was diagnosed with non-Hodgkin lymphoma.
Non-Hodgkin lymphoma, or NHL, occurs when the body produces too many abnormal leukocytes, one of the five types of white blood cells. NHL includes many different subtypes, some more aggressive than others. Survival rates average around 70% at five years and 60% at ten. Compared to some cancers, those are very hopeful numbers.
In his mid-50s and otherwise healthy, Israel began a standard chemo regimen without worrying too much. Then he sought a second opinion and his prognosis became far more serious. He switched to a more intensive chemo treatment that involved a five-day hospital stay every three weeks for round-the-clock chemo.



“I came out of that treatment in remission,” says Israel, who lives in Sammamish, not far from Seattle. “I had one more test done and thought it was just a matter of crossing my t’s and dotting my i’s. Unfortunately, the biopsy showed that the cancer was in my bone marrow. So it was back to the drawing board.”
Israel’s cancer team decided to try a stem-cell transplant, which Israel underwent in February of 2017. Of the procedures available, everyone agreed it was the least risky in terms of side effects. But a few months later, he found lumps under his arm and knew right away that the cancer was back.
After the stem-cell transplant failed, Israel had three primary choices: a donor bone-marrow transplant, CAR T-cell therapy, or palliative care. Israel was certain he didn’t want a bone-marrow transplant. While not as invasive as an organ transplant, donor blood cells can be rejected. Still a new treatment, CAR T-cell therapy also presented risks, including permanent cognitive damage. But even in the short time that had passed since Israel had first heard about it from his doctors, the experimental CAR T-cell therapy had made advances in safety and efficacy.
“My doctor told me on more than one occasion that I could decline further treatment and enjoy what time I had left,” says Israel, who at the time still had two teenage sons living at home.
“I never wanted to accept that. An 80-year-old might choose that but not me. So we went with CAR-T.”
Until recently, CAR T-cell therapy was limited to small clinical trials for patients with advanced blood cancers. In 2017, two treatments were approved by the FDA, including a therapy for adults with advanced lymphomas like Israel. He was offered a spot in a Seattle-based study before the FDA gave the treatment a green light.
CAR-T owes its name and its power to the T cell, perhaps the hardest worker of the immune system. The process is simple for the patient, starting with a blood draw. Then the patient’s T cells are separated out and biotech works its magic through genetic engineering. The new T cells produce receptors that don’t occur naturally; they’re designed to recognize and obliterate cancer cells. Once injected back in the patient, the cancer-blasting engineered T cells begin to multiply.
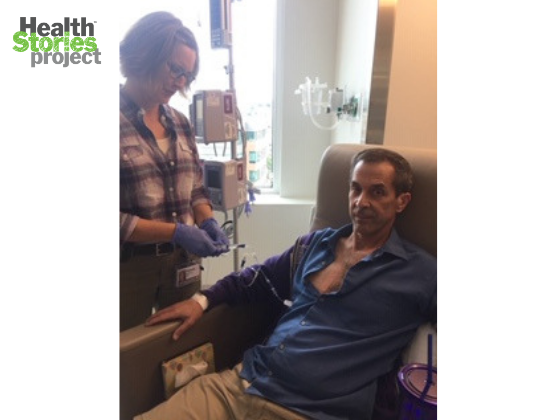
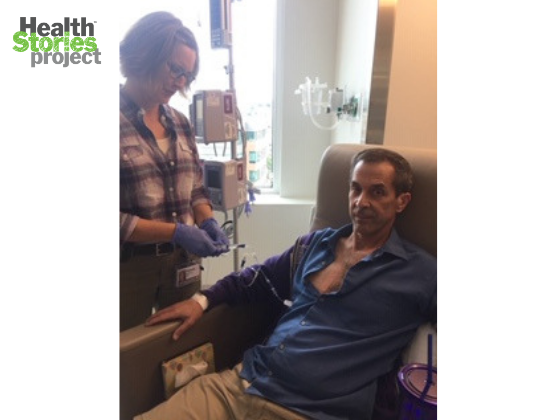
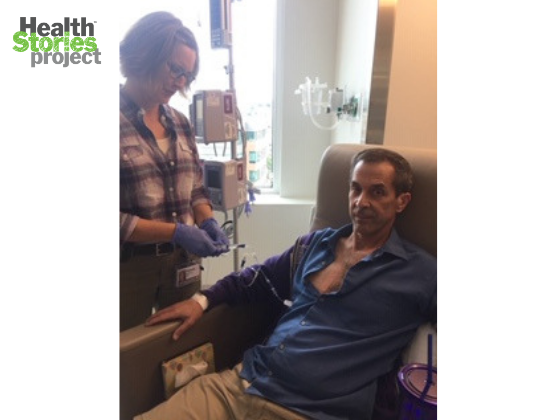
During his treatment, which lasted about a month, Israel stayed near the hospital in case of any side effects. He was admitted once during the four-week treatment for a mild fever.
“My wife was happy about this because she’d read that a fever was a sign the therapy was working,” he says.
“I was lucky and didn’t experience any of the more serious side effects. Unlike chemo, the physical burden was minimal.”
Within a week of the reinfusion of the CAR-T cells, Israel says he could feel his growths shrinking. Recently, he had his fifth clean scan subsequent to the CAR-T therapy, and won’t need another for six months. “My doctor says at this point my chances of holding remission are better than losing it,” he says. “But of course, I always have my doubts.” I’ve had five clean scans,” he says.
“It was a miracle. I might describe things a bit dispassionately now, but I’m so grateful to the doctors, the drug company, to my family, and to God.”
“I don’t take my health for granted,” he says. “A faith in a higher power has helped me through the tough days and my recovery. I wanted to live for my family, to see my two sons grow into adulthood and see the milestones in their lives. I consider myself very lucky.”
Join Us
Are you or someone you care for living with non-Hodgkin lymphoma or another health condition ? Sign up to share your experiences with others.
Latest Posts
- Living with Alzheimer’s disease
- “A Hot MS” Celebrates the Everyday Disasters That Shape Patients’ Lives
- Breast Cancer, Surgery & Recovery: There’s Nothing “Routine” About It
- “It’s OK to Not Be a Superhero”
- From “Damaged Goods” to Small Victories: Growing Up with Mental and Physical Health Conditions