It’s sudden, catastrophic, and costs our healthcare system billions of dollars every year. Sepsis, an overwhelming immune response that’s triggered by infection, strikes more than a million Americans annually. Also known as blood poisoning, sepsis spreads quickly and can lead to tissue damage, organ failure, and death. Yet far too many people know next to nothing about it.
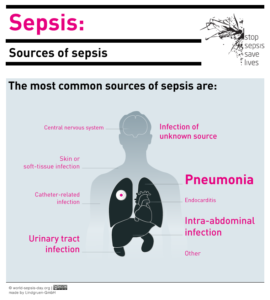
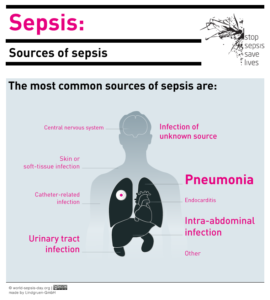
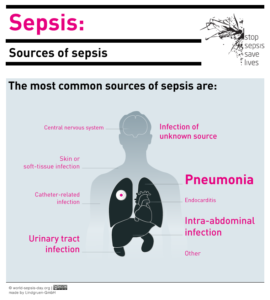
Image Source: World-Sepsis-Day.org
Sepsis happens when an infection you already have causes a chain reaction in your body. The most common types of infections linked with sepsis include the lungs (pneumonia), kidney (urinary tract infection), the gut, and the skin. Infection occurs when germs enter the body and multiply, causing illness. Germs that can cause infections leading to sepsis include staph, E. coli, and some forms of strep.
Most of the time, a healthy body is able to fight off infection on its own or with basic antibiotics. Sometimes, however, the immune chemicals released into the blood to deal with infection can trigger widespread inflammation, leading to blood clots and leaky vessels. Impaired blood flow deprives organs of vital oxygen and nutrients. In the worst cases, blood pressure drops precipitously, the heart weakens, and multiple organs fail. More than 250,000 Americans die from septic shock every year-that’s one person every two minutes.
While anybody can contract an infection that leads to sepsis, certain groups are at a much higher risk, including infants, adults over 65, people with chronic diseases, and those with compromised immune systems. According to the CDC, seven in 10 patients diagnosed with sepsis recently received healthcare services or have chronic conditions requiring frequent medical care. It occasionally occurs in young, healthy people, as well.
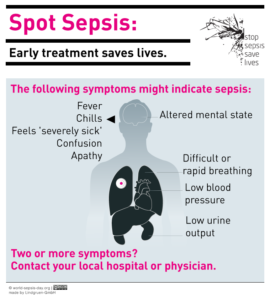
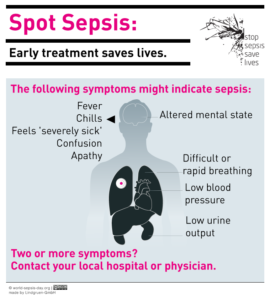
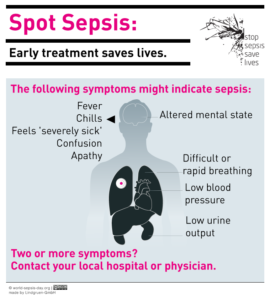
Image Source: World-Sepsis-Day.org
What makes sepsis particularly scary is that it’s not simple to diagnose. Doctors look for fever, increased heart rate, increased respiratory rate, and abnormal white blood cell counts. They also test blood, urine, and sputum for infectious agents. When it comes to sepsis, every minute counts; the sooner it’s caught, the better the outcome with aggressive treatment. Unfortunately, sepsis often isn’t detected until it’s too late. Many medical researchers are searching for ways to recognize sepsis easily in the very earliest stages.
In the meantime, the most important way to protect against sepsis is through awareness. We’ve listed a few useful tips below, and you can find much more detailed information – as well as stories from both survivors and families who’ve lost loved ones to sepsis – online at the CDC ), the NIH, and Sepsis Alliance.
Prevent Infection
This may sound like a no-brainer, but always wash your hands and even make use of Hand Sanitizer products to completely cleanse your hands and wrists of any infections or bacteria. You’ll be wanting to keep an eye on visible skin infections, even something as small as a bug bite or splinter. Make sure you receive recommended vaccines, such as flu and pneumococcal, especially if you are in a high-risk group.
Watch for Symptoms
Be on the lookout for the following symptoms, particularly if you’ve recently received medical treatment for an infection or have a chronic disease.
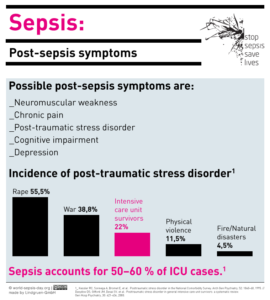
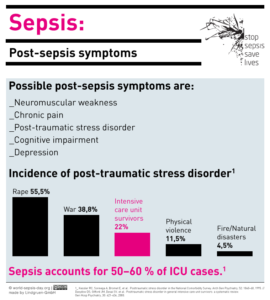
Image Source: World-Sepsis-Day.org
Symptoms are often mistaken for a severe case of the flu at first. Don’t take any chances if you or a family member experiences the following:
- Shivering, fever, or very cold
- Extreme pain or discomfort
- Clammy, sweaty, or mottled skin
- Confusion, disorientation, or slurred speech
- No passing of urine in a day
- Shortness of breath
- High heart rate
Advocate for Yourself
If you suspect sepsis, see a healthcare professional immediately. Be very thorough when disclosing your medical history and current symptoms. Specifically mention sepsis as a concern. Remember, the earlier it’s caught, the more likely you are to survive, so advocate for yourself. Ask questions, request tests, and see another doctor if you don’t feel you’ve been taken seriously. It’s a matter of life and death, after all.